When adults go through trauma, it can leave deep emotional scars. People with trauma or PTSD (Post-Traumatic Stress Disorder) often feel intense emotions. They may experience flashbacks, panic, and a constant sense of danger, even when the trauma is over.
If you have PTSD, you might notice some or all of these symptoms:
| PTSD SYMPTOM | WHAT IT FEELS LIKE |
| Flashbacks | Feeling like the trauma is happening all over again |
| Nightmares | Bad dreams about the trauma or other scary things |
| Avoidance | Staying away from places, people, or memories |
| Feeling on edge | Always alert, easily startled, trouble relaxing |
| Negative thoughts and feelings | Feeling hopeless, guilty, or disconnected from others |
| Memory problems | Trouble remembering parts of the trauma |
| Trouble Sleeping | Hard time fallijng asleep or staying asleep |
| Anger or irritability | Getting angry easily or feeling frustrated a lot |
PTSD can affect every part of daily life. It can make it harder to trust people, focus at work or school, or even enjoy things you once loved.
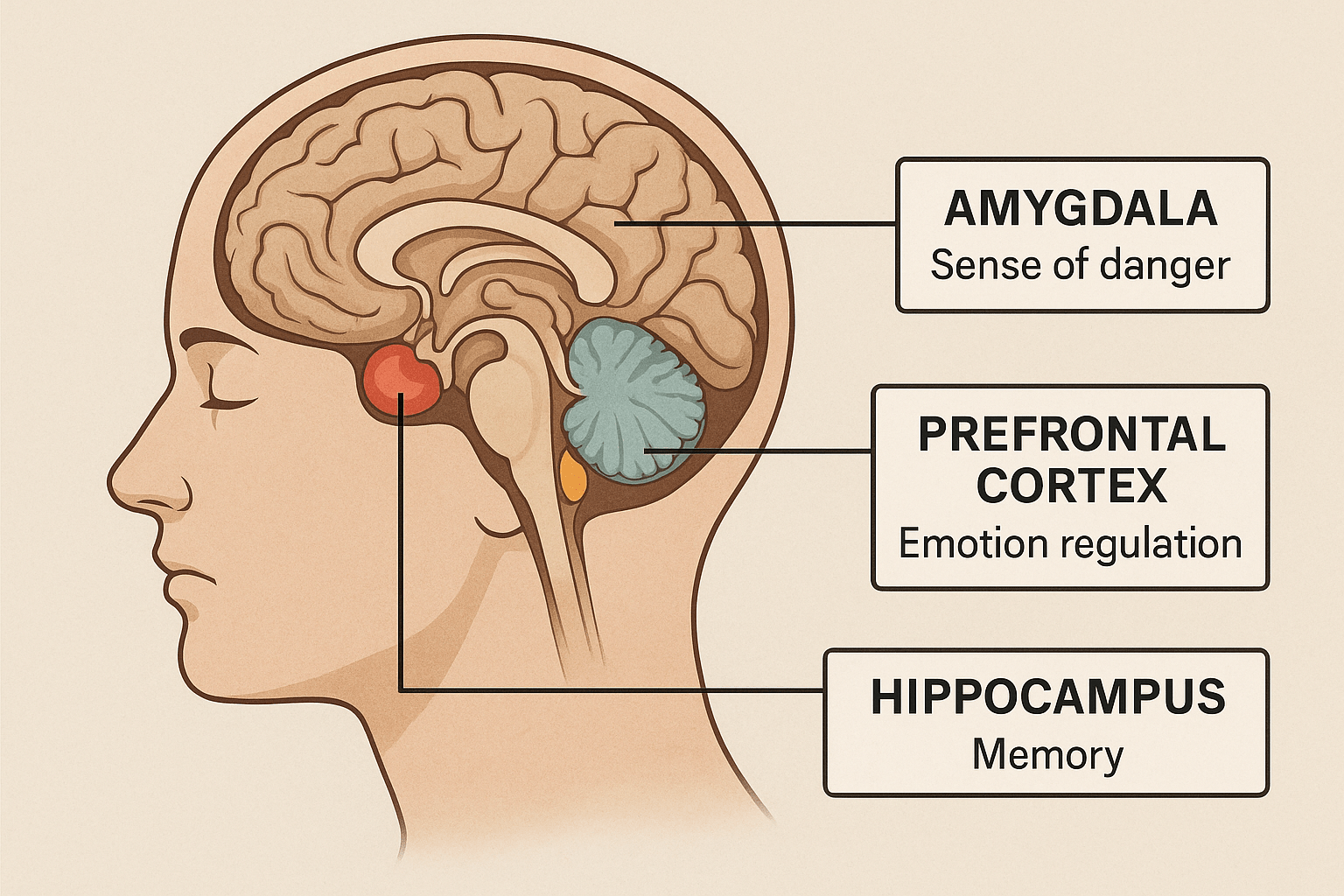
The trauma may have occurred when you were a child and affected your social and brain development. Childhood trauma can have lasting effects through adulthood. It impacts brain development and daily functioning. When someone experiences trauma, their brain shifts into survival mode. The amygdala and other brain parts that sense danger become overactive. This means that even when a person is safe, their brain might still act like they’re in danger. The prefrontal cortex helps us make decisions and manage emotions. When it becomes underactive, we might find it hard to think clearly or stay calm during stress. The hippocampus helps with memory and separates past from present. It may shrink, which can lead to flashbacks or feeling “stuck” in trauma.
How Trauma Affects the Brain
For children, trauma can interrupt normal brain development. Kids who grow up in unsafe or unpredictable places often struggle. They may have trouble with attention, learning, making friends, and managing their feelings. Their nervous systems might stay in a constant “high alert” mode. This makes it hard to feel safe, connected, or focused. In adulthood, this may lead to chronic anxiety, trust issues, mood swings, or feeling “on edge.”
Healing from trauma is tough. These patterns are deeply wired into our brain and body. Trauma recovery means helping the nervous system feel safe again. This process takes time and patience. Therapy is not just about talking about trauma. It helps people build skills to manage strong emotions. These include grounding, breathing, mindfulness, and recognizing what triggers the brain’s danger response. That’s why effective trauma treatment moves slowly and with care. Healing from PTSD takes time, but with the right therapy and support, it is possible to feel safe, connected, and hopeful again.
If you are struggling with PTSD symptoms, reaching out for help is a strong and important first step. But it needs to be the right help. And it’s important to be prepared for the work you’ll do in trauma treatment, so it can be effective.
Steps in Trauma Recovery: How People Heal from PTSD and Emotional Trauma
Healing from trauma takes time, but recovery is possible. Many people who have been through trauma or PTSD (Post-Traumatic Stress Disorder) go through several steps in their healing journey. These steps help people feel safer, manage their emotions, and start living again without being stuck in the past.
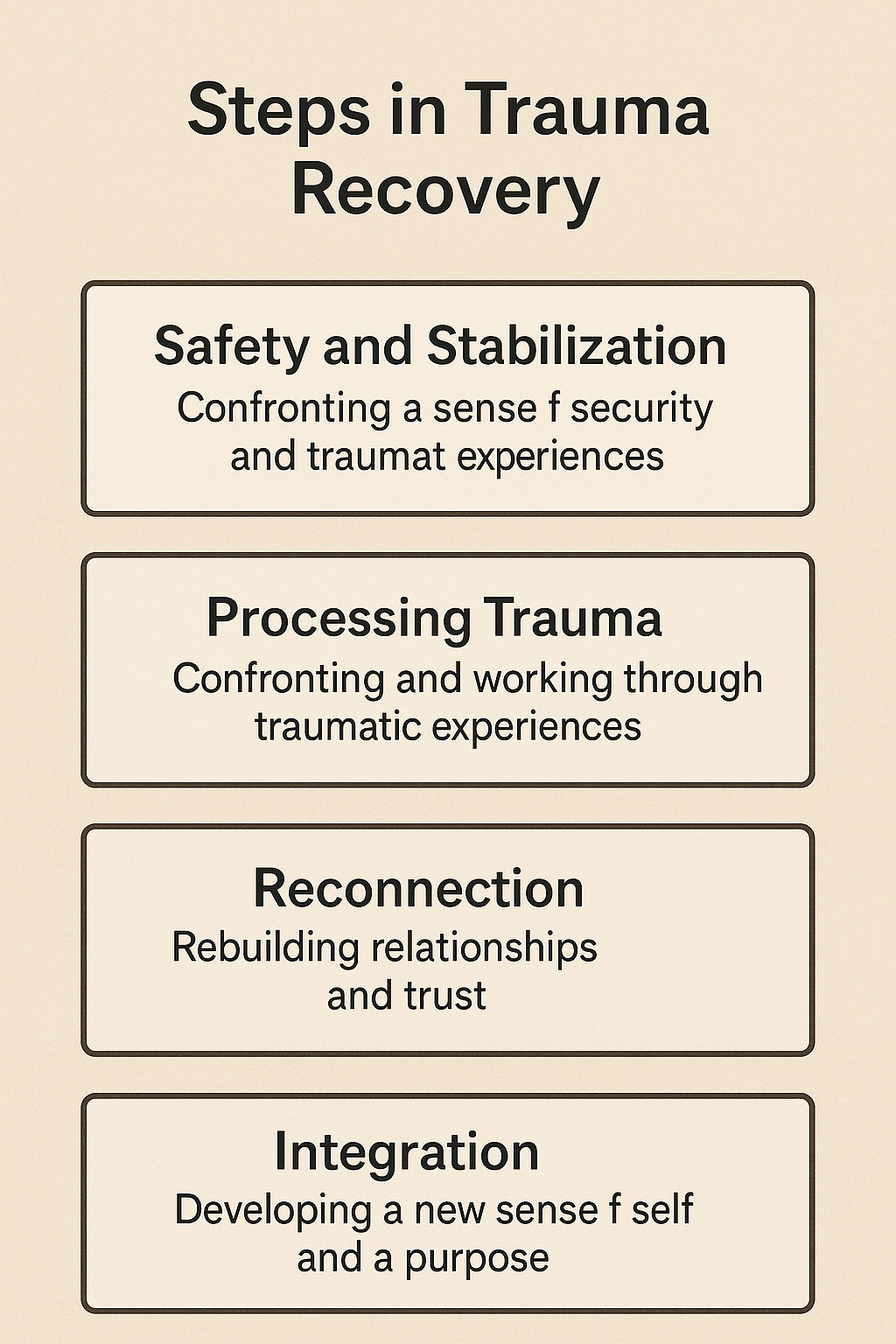
1. Feeling Safe Again
The first step in healing from trauma is learning how to feel safe. After trauma, the brain can stay in “danger mode,” even when nothing bad is happening. Healing from trauma is a journey, and the very first step is learning how to feel safe again. After experiencing trauma, the brain can get stuck in what’s known as “danger mode.” This is the brain’s way of protecting you, but it can continue long after the threat is gone.
When your brain stays in this survival state, it constantly scans for danger—even in situations that are actually safe. This can lead to symptoms like anxiety, jumpiness, trouble sleeping, and difficulty trusting others. You might feel like you’re always on edge, waiting for something bad to happen. These are common signs of post-traumatic stress, and they’re your brain’s way of saying, “Something’s not right.”
Because of this, trauma recovery can’t start with talking about what happened right away. First, the body and mind need to learn how to calm down and feel secure. Therapists often call this “building safety and stability.” It’s the foundation for all other healing.
Some examples of ways to begin building safety include:
- Practicing grounding techniques to stay in the present moment
- Creating a routine that brings structure and predictability
- Spending time with supportive people who help you feel calm
- Learning breathing exercises or mindfulness skills to reduce anxiety
- Working with a trauma-informed therapist who understands how trauma affects the nervous system
Once a person feels safer in their body and environment, they’re better able to process painful memories and build healthier relationships. Trying to dive into trauma work too soon—without first feeling safe—can actually be re-traumatizing.
Feeling safe doesn’t mean nothing bad will ever happen again. It means trusting that you have the tools to handle what comes your way. That sense of safety is the foundation of all meaningful trauma recovery.
This makes it hard to relax or trust others. In trauma therapy, people learn simple tools to help calm their bodies and minds.
2. Learning to Handle Strong Emotions
Many people with PTSD feel big emotions like fear, sadness, anger, or shame. A big part of recovery is learning how to handle these emotions without letting them take over.
Many people begin to process what happened to them in this second step and how it affected their emotions. If you have PTSD, strong emotions like fear, sadness, anger, or shame and come out of nowhere and may feel overwhelming or even scary. Sometimes they don’t match the situation you’re in—like getting really angry over something small or feeling sad when nothing seems wrong.
This part of healing is about learning how to face those feelings instead of pushing them away or letting them control you. It’s normal to want to avoid painful emotions, but avoiding them can make them even stronger later. Trauma treatment helps people learn tools to safely feel their emotions, understand where they come from, and find healthy ways to respond.
What Processing Looks Like
In therapy, this step may include:
- Naming emotions – learning to notice and describe what you’re feeling
- Mindfulness – staying present without getting swept away by emotion
- Grounding techniques – like holding a cold object or describing your surroundings out loud to bring your focus back to the present
- Validation – learning to tell yourself, “It makes sense I feel this way,” instead of judging yourself
Example:
Let’s say you were in a car accident. Months later, you might feel terrified just sitting in a car—even if you know you’re safe. Processing means understanding that fear and working through it, rather than avoiding cars forever or forcing yourself to pretend you’re not afraid.
You Are Not Broken
Big feelings are not a sign that you’re weak or broken—they are signs that your body and brain are still reacting to something painful. Learning how to process emotions gives you back a sense of control. Instead of feeling trapped by your feelings, you start to feel stronger and more prepared.
3. Talking About the Trauma (When You’re Ready)
After someone feels more in control of their emotions, they can begin to talk about what happened. This is a slow, gentle process. Therapists use special methods like EMDR or CPT to help people face their memories without feeling overwhelmed.
Example: In a therapy session, you might talk about a memory while using tapping or eye movements to help your brain feel safe and strong while remembering. You could also use the DBT skills you have learned.
4. Rebuilding Your Life (Integration)
As people heal, they start to feel more like themselves again. They may rebuild relationships, try new hobbies, or feel more confident in everyday life. Recovery doesn’t mean forgetting the trauma—it means learning to live with it in a way that doesn’t control you anymore.
Example: You might start making plans for the future, spending more time with friends, or going back to school or work
Recovery is rarely a straight line. Feelings often get more intense before they get better, which can be discouraging. That’s why trauma treatment needs to be done with care. Before talking about what happened, a person needs skills to handle tough emotions. With the right support, people can change their brains. They can form new patterns and start living with more ease and connection. This is where DBT (Dialectical Behavior Therapy) can help.
In Adult Intensive Outpatient Programs (IOPs), DBT helps people gain control over their emotions. This support allows them to heal safely. Let’s explore how DBT supports trauma recovery in IOP programs and why it’s such an important part of treatment.
DBT is a type of therapy that teaches people how to:
- Stay calm during stress
- Understand and manage emotions
- Improve relationships
- Be more aware of the present moment
It was first created for people with strong, hard-to-control emotions. But now, it is used to help people with many mental health concerns—including trauma and PTSD.
Why You Need DBT Skills Before Trauma Therapy
Healing from trauma often brings up painful emotions. People may feel sadness, fear, anger, guilt, or shame. Trauma therapy can be tough. It feels overwhelming when someone doesn’t have the skills to handle these feelings.
Example: Imagine someone starts talking about a past assault in therapy. They begin to feel panic, start crying, and feel like they want to run out of the room or dissociate. Without ways to relax, they may skip therapy or resort to unhealthy habits, like drinking or self-harm. At worst they could be more traumatized.
With DBT skills, they could instead:
- Use mindfulness to take deep breaths and notice their body
- Practice self-soothing, like holding a soft blanket or listening to calming music
- Use grounding techniques
- Use a Distress Toleranceskill, like going for a walk or calling a support person
These tools help people feel more grounded and able to continue therapy.
What Skills Does DBT Teach?
In an adult IOP program, DBT teaches four main skill sets:
- Mindfulness:Learn to stay in the moment. This helps people notice their thoughts and feelings without getting overwhelmed. Example: “I notice I’m feeling anxious, and I can take deep breaths to calm down.”
- Distress Tolerance:Learn how to survive emotional pain without making things worse. Learn how to use your senses for self-soothing and comfort. Learn how to get into a state of safety. For example, try the 5-4-3-2-1 grounding technique.
- Emotion Regulation:Understand emotions and how to manage them in healthy ways. Learn the triggers for your emotions. Discover how your emotions connect to your physical sensations. Eat regular meals and get enough sleep. This helps reduce emotional ups and downs.
- Interpersonal Effectiveness:Build stronger relationships and learn to set boundaries. Example: Saying “no” kindly or asking for support without guilt.
DBT in IOP: A Safe Start to Trauma Recovery
An Intensive Outpatient Program (IOP) is a great place to learn DBT skills. In an IOP, clients come to therapy several days a week. This structure gives people time to learn and practice skills in real life.
Feeling confident in DBT tools usually means a person ready for trauma-focused therapy. This includes EMDR, DBT-PE, or Prolonged Exposure. With DBT, they already know how to manage the hard feelings that come up during trauma work.
Before starting trauma therapy, a person could use DBT skills to create a coping plan, such as:
- Call my support person after session
- Use skills to stay present
- Separate the trauma response from what is actually happening now
- Take a walk after therapy
- Use my “Coping Skills Box” with calming tools
Healing from Trauma Takes Time—and Tools
Trauma affects more than the brain. It also impacts the body, emotions, and relationships. DBT gets this. It helps people gain skills to feel safe, stick with therapy, and start healing.
Healing from PTSD or trauma is not easy. Sometimes things feel worse before they get better. But with the right support, therapy, and tools, people can feel safe, calm, and strong again. You are not alone, and recovery is possible
In adult IOP programs, DBT helps trauma survivors feel strong and in control. It’s a step-by-step path to healing, and no one has to take that path alone.
Looking for Trauma Therapy with DBT? If you or a loved one is looking for a trauma-informed IOP that uses DBT, our team can help. Contact us today to see how our program helps recovery. We focus on compassion, structure, and real-life skills.

